Ocracokers worry about the future of Emergency Medical Services on the island
Editor’s note: This is the first in a series of articles on the financial problems in the Hyde County Department of Emergency Services, which will directly affect Ocracoke in some manner. The Island Free Press will run more articles as the attempts to avert a crisis continue.)
After a special work session and two public meetings, the Hyde County commissioners are still working on a solution to their quest to reduce the emergency medical services budget.
A presentation on the EMS by paramedics Brian Carter and Jeff Hibbard at a special meeting Sept. 22, while informative, did not provide all of the information the commissioners sought.
Carter, though not the overall EMS director, described the differences in what basic emergency medical technicians (EMTs), intermediate EMTs, and the more advanced paramedics do and the costs incurred during an emergency call.
He also presented budget and staffing scenarios for all three levels of service separately.
Hyde County is currently without an EMS director.
One of the issues is the increased cost of having paramedic-level service for the entire county, which was put into effect in 2009. Before that, only Ocracoke Island had paramedics, while the rest of Hyde County had basic- and intermediate-level EMTs.
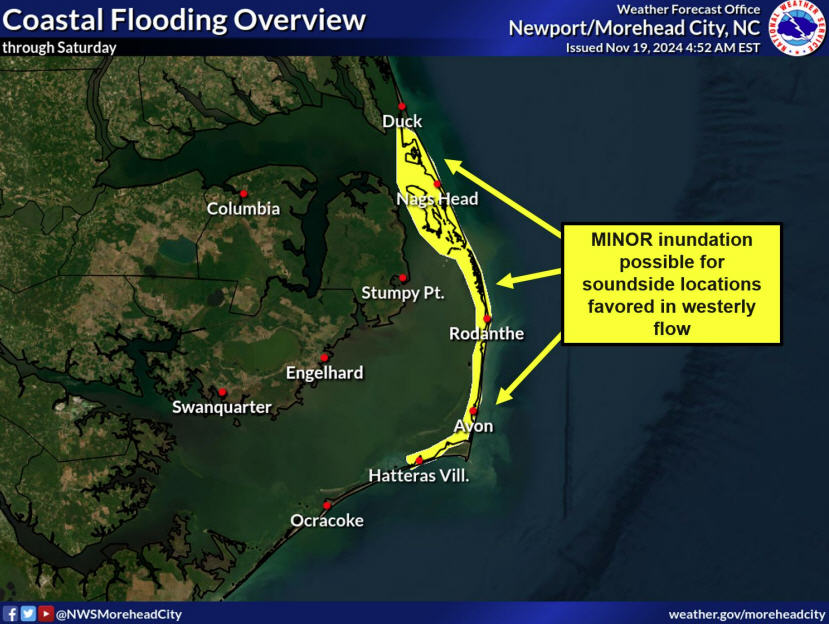
Paramedic service began on the island in 2003 when the Federal Emergency Management Agency sent a paramedic crew to Ocracoke after Hurricane Isabel cut an inlet between Hatteras and Frisco, basically leaving long ferry rides to the mainland as the only route off the island. Paramedics were needed on Ocracoke to provide emergency care while waiting for air ambulances, which was the only way of transporting patients off the island.
Cheryl Ballance of the Ocracoke Health Center was instrumental in retaining paramedic service on the island, and the OHC contracted for it and was reimbursed by the county. Hyde County took over the EMS service in December of 2007.
Before 2009, the entire EMS expense budget was $928,672. The estimated total EMS expense for 2010, as of April 30, was $1,430,916, according to the most recent budget online at www.hydecounty.org.
The current budget includes $1,578,141 in EMS expenses. At the end of Carter’s presentation, his numbers showed a savings of about $30,000 against the approved budget amount.
Commissioner Sharon Spencer noted that in the spring, the then-director of the EMS had asked the board for an additional $364,000 to fund the program to the end of the fiscal year.
“We are pleased to have paramedic care, but can we afford it?” she asked. “Will we get these requests (for more money) every year?”
Included in the total budget is $190,000 in overtime pay. Carter noted that they’ve already spent 25 percent of that. Current full-time salary expenditures are at 13 percent and part-time are 20 percent. Salary figures are $705,000 for full-time staff and $90,000 for part-time.
Another issue is whether better scheduling can reduce overtime. The board discussed at length the disparity between the part-time and full-time staff budgets and whether hiring more full-time staff would reduce overtime.
Better collection on billing would also help the coffers. The current collection rate is 42 percent of billing, which is done by county employees.
David M. Smitherman, interim county manager, noted that he is looking into the costs of outsourcing billing, which might yield a better collection rate. Billing had been outsourced but was brought back in-house in 2009.
According to Carter, last year $701,000 was billed and $252,009 of that was collected, leaving an uncollected balance of $448,991.
The shortfall results mostly from Medicare and Medicaid paying only a fraction of what each emergency run actually costs, which Smitherman said is $859. Medicare and Medicaid reimbursement rates change quarterly, he said, and these agencies will only pay up to 80 percent of what is billed, never 100 percent.
“Right off the bat, we’ll always have a 20 percent write-off from revenues,” he said.
Moreover, no one reimburses the county for the 400-plus responses that don’t result in transport to a medical facility.
On hand also at this special meeting on the EMS service was Allen Johnson, a regional specialist with the Office of Emergency Medical Services of the North Carolina Department of Health and Human Services, which is a regulatory agency and does not set policy.
“You are in a unique situation here,” he noted. “You had paramedic-level service on Ocracoke and then had to provide the same level of service to the entire county.”
While other North Carolina counties’ emergency trips to the hospital are eight to 10 minutes, Hyde County’s average is 35 minutes or more, he noted. During these longer trips, “paramedics can actually see medications working on the way to the hospital,” he said.
Another situation that must be considered is that the Ocracoke Health Center is a family practice for residents of the island, IGC administrative director Cheryl Ballance explained. Although it is not a critical care facility, it treats everyone who walks through the door, with many critical emergencies immediately referred to the EMTs in the building behind the health center. Though fewer than 1,000 people live on the island, the population swells to thousands in the summer. Caring for the summer visitors can be a strain on the facility, but it also generates income for the practice.
At an Aug. 19 county board meeting, a comment was made that paramedic service on Ocracoke might have to be discontinued, said Cheryl Ballance, who said she was “shocked” by the idea.
More recent suggestions have included keeping paramedics on Ocracoke and using the basic and intermediate EMTs in the rest of the county.
Johnson said if the final decision is to retain paramedic-level service only on Ocracoke and a lower level on the mainland, this would require a recertification issued by the state. Smitherman thinks this could be accomplished before the end of the fiscal year.
While members of the public who attended this special meeting were not allowed to comment, they were allowed to do so during the regular Board of Commissioners’ meeting held immediately after the EMS work session.
Among those who spoke was the new doctor at Ocracoke Health Center (OHC), Dr. Erin Baker, who joined the staff this summer.
“I took this position knowing there would be paramedic-level care,” she said. “I am a family practice doctor and not qualified to intubate.”
Soon after she began, she had a case that required an airway opened and the helicopter was out of commission, Baker said. “I was so thankful a paramedic was here to accompany the patient to the hospital,” she said. “Eliminating paramedics here would be a step backwards.”
Gail Covington, the recently re-hired nurse-practitioner at the OHC, said she had worked here 15 years ago when there was only basic EMT-level care. She urged the commissioners to explore better scheduling.
“One of my reasons to come back was paramedic-level care,” she said. “There are increasing numbers of boaters having paramedic-level accidents. We had a drowning and three near-drownings where paramedics were needed.”
Cheryl Ballance, administrative director of the OHC, said if the EMS service was reduced from paramedic-level it would affect all the citizens.
“Of the 103 paramedic calls we had, at least 50 percent originated from the health center,” she said. “We’re here to serve the citizens. (The county providing) health services to the community is so important.”
Leslie Lanier, owner of Books to be Read, testified that it is two and a half hours from Ocracoke to a hospital (via ambulance).
“We’ll be remiss if we go to a lower level of service,” she said. “We have thousands of visitors with anything from a hangnail to a shark attack. We need to get overtime under control, which needs a strong manager.”
At the Monday, Oct. 4 regular meeting, the commissioners again talked about the need to have more solid figures about the true costs and revenues of paramedic-level service vs. a lower level.
At one point, commissioner Anson Byrd said, “Ocracoke is a unique situation. Perhaps we can have basic and intermediate services on the mainland and leave paramedic-level on Ocracoke.”
They commissioners decided to have another special meeting on Oct. 18 to rehash the numbers at 3:30 p.m. before the regular board meeting at 7 p.m.
(Connie Leinbach’s career has included jobs as a daily newspaper journalist and freelancer. She now owns a home on Ocracoke, where she hopes to spend most of her time. She is a reporter for the Ocracoke Observer.)
Editor’s note: This is the first in a series of articles on the financial problems in the Hyde County Department of Emergency Services, which will directly affect Ocracoke in some manner. The Island Free Press will run more articles as the attempts to avert a crisis continue.)
After a special work session and two public meetings, the Hyde County commissioners are still working on a solution to their quest to reduce the emergency medical services budget.
A presentation on the EMS by paramedics Brian Carter and Jeff Hibbard at a special meeting Sept. 22, while informative, did not provide all of the information the commissioners sought.
Carter, though not the overall EMS director, described the differences in what basic emergency medical technicians (EMTs), intermediate EMTs, and the more advanced paramedics do and the costs incurred during an emergency call.
He also presented budget and staffing scenarios for all three levels of service separately.
Hyde County is currently without an EMS director.
One of the issues is the increased cost of having paramedic-level service for the entire county, which was put into effect in 2009. Before that, only Ocracoke Island had paramedics, while the rest of Hyde County had basic- and intermediate-level EMTs.
Paramedic service began on the island in 2003 when the Federal Emergency Management Agency sent a paramedic crew to Ocracoke after Hurricane Isabel cut an inlet between Hatteras and Frisco, basically leaving long ferry rides to the mainland as the only route off the island. Paramedics were needed on Ocracoke to provide emergency care while waiting for air ambulances, which was the only way of transporting patients off the island.
Cheryl Ballance of the Ocracoke Health Center was instrumental in retaining paramedic service on the island, and the OHC contracted for it and was reimbursed by the county. Hyde County took over the EMS service in December of 2007.
Before 2009, the entire EMS expense budget was $928,672. The estimated total EMS expense for 2010, as of April 30, was $1,430,916, according to the most recent budget online at www.hydecounty.org.
The current budget includes $1,578,141 in EMS expenses. At the end of Carter’s presentation, his numbers showed a savings of about $30,000 against the approved budget amount.
Commissioner Sharon Spencer noted that in the spring, the then-director of the EMS had asked the board for an additional $364,000 to fund the program to the end of the fiscal year.
“We are pleased to have paramedic care, but can we afford it?” she asked. “Will we get these requests (for more money) every year?”
Included in the total budget is $190,000 in overtime pay. Carter noted that they’ve already spent 25 percent of that. Current full-time salary expenditures are at 13 percent and part-time are 20 percent. Salary figures are $705,000 for full-time staff and $90,000 for part-time.
Another issue is whether better scheduling can reduce overtime. The board discussed at length the disparity between the part-time and full-time staff budgets and whether hiring more full-time staff would reduce overtime.
Better collection on billing would also help the coffers. The current collection rate is 42 percent of billing, which is done by county employees.
David M. Smitherman, interim county manager, noted that he is looking into the costs of outsourcing billing, which might yield a better collection rate. Billing had been outsourced but was brought back in-house in 2009.
According to Carter, last year $701,000 was billed and $252,009 of that was collected, leaving an uncollected balance of $448,991.
The shortfall results mostly from Medicare and Medicaid paying only a fraction of what each emergency run actually costs, which Smitherman said is $859. Medicare and Medicaid reimbursement rates change quarterly, he said, and these agencies will only pay up to 80 percent of what is billed, never 100 percent.
“Right off the bat, we’ll always have a 20 percent write-off from revenues,” he said.
Moreover, no one reimburses the county for the 400-plus responses that don’t result in transport to a medical facility.
On hand also at this special meeting on the EMS service was Allen Johnson, a regional specialist with the Office of Emergency Medical Services of the North Carolina Department of Health and Human Services, which is a regulatory agency and does not set policy.
“You are in a unique situation here,” he noted. “You had paramedic-level service on Ocracoke and then had to provide the same level of service to the entire county.”
While other North Carolina counties’ emergency trips to the hospital are eight to 10 minutes, Hyde County’s average is 35 minutes or more, he noted. During these longer trips, “paramedics can actually see medications working on the way to the hospital,” he said.
Another situation that must be considered is that the Ocracoke Health Center is a family practice for residents of the island, IGC administrative director Cheryl Ballance explained. Although it is not a critical care facility, it treats everyone who walks through the door, with many critical emergencies immediately referred to the EMTs in the building behind the health center. Though fewer than 1,000 people live on the island, the population swells to thousands in the summer. Caring for the summer visitors can be a strain on the facility, but it also generates income for the practice.
At an Aug. 19 county board meeting, a comment was made that paramedic service on Ocracoke might have to be discontinued, said Cheryl Ballance, who said she was “shocked” by the idea.
More recent suggestions have included keeping paramedics on Ocracoke and using the basic and intermediate EMTs in the rest of the county.
Johnson said if the final decision is to retain paramedic-level service only on Ocracoke and a lower level on the mainland, this would require a recertification issued by the state. Smitherman thinks this could be accomplished before the end of the fiscal year.
While members of the public who attended this special meeting were not allowed to comment, they were allowed to do so during the regular Board of Commissioners’ meeting held immediately after the EMS work session.
Among those who spoke was the new doctor at Ocracoke Health Center (OHC), Dr. Erin Baker, who joined the staff this summer.
“I took this position knowing there would be paramedic-level care,” she said. “I am a family practice doctor and not qualified to intubate.”
Soon after she began, she had a case that required an airway opened and the helicopter was out of commission, Baker said. “I was so thankful a paramedic was here to accompany the patient to the hospital,” she said. “Eliminating paramedics here would be a step backwards.”
Gail Covington, the recently re-hired nurse-practitioner at the OHC, said she had worked here 15 years ago when there was only basic EMT-level care. She urged the commissioners to explore better scheduling.
“One of my reasons to come back was paramedic-level care,” she said. “There are increasing numbers of boaters having paramedic-level accidents. We had a drowning and three near-drownings where paramedics were needed.”
Cheryl Ballance, administrative director of the OHC, said if the EMS service was reduced from paramedic-level it would affect all the citizens.
“Of the 103 paramedic calls we had, at least 50 percent originated from the health center,” she said. “We’re here to serve the citizens. (The county providing) health services to the community is so important.”
Leslie Lanier, owner of Books to be Read, testified that it is two and a half hours from Ocracoke to a hospital (via ambulance).
“We’ll be remiss if we go to a lower level of service,” she said. “We have thousands of visitors with anything from a hangnail to a shark attack. We need to get overtime under control, which needs a strong manager.”
At the Monday, Oct. 4 regular meeting, the commissioners again talked about the need to have more solid figures about the true costs and revenues of paramedic-level service vs. a lower level.
At one point, commissioner Anson Byrd said, “Ocracoke is a unique situation. Perhaps we can have basic and intermediate services on the mainland and leave paramedic-level on Ocracoke.”
They commissioners decided to have another special meeting on Oct. 18 to rehash the numbers at 3:30 p.m. before the regular board meeting at 7 p.m.
(Connie Leinbach’s career has included jobs as a daily newspaper journalist and freelancer. She now owns a home on Ocracoke, where she hopes to spend most of her time. She is a reporter for the Ocracoke Observer.)
Editor’s note: This is the first in a series of articles on the financial problems in the Hyde County Department of Emergency Services, which will directly affect Ocracoke in some manner. The Island Free Press will run more articles as the attempts to avert a crisis continue.)
After a special work session and two public meetings, the Hyde County commissioners are still working on a solution to their quest to reduce the emergency medical services budget.
A presentation on the EMS by paramedics Brian Carter and Jeff Hibbard at a special meeting Sept. 22, while informative, did not provide all of the information the commissioners sought.
Carter, though not the overall EMS director, described the differences in what basic emergency medical technicians (EMTs), intermediate EMTs, and the more advanced paramedics do and the costs incurred during an emergency call.
He also presented budget and staffing scenarios for all three levels of service separately.
Hyde County is currently without an EMS director.
One of the issues is the increased cost of having paramedic-level service for the entire county, which was put into effect in 2009. Before that, only Ocracoke Island had paramedics, while the rest of Hyde County had basic- and intermediate-level EMTs.
Paramedic service began on the island in 2003 when the Federal Emergency Management Agency sent a paramedic crew to Ocracoke after Hurricane Isabel cut an inlet between Hatteras and Frisco, basically leaving long ferry rides to the mainland as the only route off the island. Paramedics were needed on Ocracoke to provide emergency care while waiting for air ambulances, which was the only way of transporting patients off the island.
Cheryl Ballance of the Ocracoke Health Center was instrumental in retaining paramedic service on the island, and the OHC contracted for it and was reimbursed by the county. Hyde County took over the EMS service in December of 2007.
Before 2009, the entire EMS expense budget was $928,672. The estimated total EMS expense for 2010, as of April 30, was $1,430,916, according to the most recent budget online at www.hydecounty.org.
The current budget includes $1,578,141 in EMS expenses. At the end of Carter’s presentation, his numbers showed a savings of about $30,000 against the approved budget amount.
Commissioner Sharon Spencer noted that in the spring, the then-director of the EMS had asked the board for an additional $364,000 to fund the program to the end of the fiscal year.
“We are pleased to have paramedic care, but can we afford it?” she asked. “Will we get these requests (for more money) every year?”
Included in the total budget is $190,000 in overtime pay. Carter noted that they’ve already spent 25 percent of that. Current full-time salary expenditures are at 13 percent and part-time are 20 percent. Salary figures are $705,000 for full-time staff and $90,000 for part-time.
Another issue is whether better scheduling can reduce overtime. The board discussed at length the disparity between the part-time and full-time staff budgets and whether hiring more full-time staff would reduce overtime.
Better collection on billing would also help the coffers. The current collection rate is 42 percent of billing, which is done by county employees.
David M. Smitherman, interim county manager, noted that he is looking into the costs of outsourcing billing, which might yield a better collection rate. Billing had been outsourced but was brought back in-house in 2009.
According to Carter, last year $701,000 was billed and $252,009 of that was collected, leaving an uncollected balance of $448,991.
The shortfall results mostly from Medicare and Medicaid paying only a fraction of what each emergency run actually costs, which Smitherman said is $859. Medicare and Medicaid reimbursement rates change quarterly, he said, and these agencies will only pay up to 80 percent of what is billed, never 100 percent.
“Right off the bat, we’ll always have a 20 percent write-off from revenues,” he said.
Moreover, no one reimburses the county for the 400-plus responses that don’t result in transport to a medical facility.
On hand also at this special meeting on the EMS service was Allen Johnson, a regional specialist with the Office of Emergency Medical Services of the North Carolina Department of Health and Human Services, which is a regulatory agency and does not set policy.
“You are in a unique situation here,” he noted. “You had paramedic-level service on Ocracoke and then had to provide the same level of service to the entire county.”
While other North Carolina counties’ emergency trips to the hospital are eight to 10 minutes, Hyde County’s average is 35 minutes or more, he noted. During these longer trips, “paramedics can actually see medications working on the way to the hospital,” he said.
Another situation that must be considered is that the Ocracoke Health Center is a family practice for residents of the island, IGC administrative director Cheryl Ballance explained. Although it is not a critical care facility, it treats everyone who walks through the door, with many critical emergencies immediately referred to the EMTs in the building behind the health center. Though fewer than 1,000 people live on the island, the population swells to thousands in the summer. Caring for the summer visitors can be a strain on the facility, but it also generates income for the practice.
At an Aug. 19 county board meeting, a comment was made that paramedic service on Ocracoke might have to be discontinued, said Cheryl Ballance, who said she was “shocked” by the idea.
More recent suggestions have included keeping paramedics on Ocracoke and using the basic and intermediate EMTs in the rest of the county.
Johnson said if the final decision is to retain paramedic-level service only on Ocracoke and a lower level on the mainland, this would require a recertification issued by the state. Smitherman thinks this could be accomplished before the end of the fiscal year.
While members of the public who attended this special meeting were not allowed to comment, they were allowed to do so during the regular Board of Commissioners’ meeting held immediately after the EMS work session.
Among those who spoke was the new doctor at Ocracoke Health Center (OHC), Dr. Erin Baker, who joined the staff this summer.
“I took this position knowing there would be paramedic-level care,” she said. “I am a family practice doctor and not qualified to intubate.”
Soon after she began, she had a case that required an airway opened and the helicopter was out of commission, Baker said. “I was so thankful a paramedic was here to accompany the patient to the hospital,” she said. “Eliminating paramedics here would be a step backwards.”
Gail Covington, the recently re-hired nurse-practitioner at the OHC, said she had worked here 15 years ago when there was only basic EMT-level care. She urged the commissioners to explore better scheduling.
“One of my reasons to come back was paramedic-level care,” she said. “There are increasing numbers of boaters having paramedic-level accidents. We had a drowning and three near-drownings where paramedics were needed.”
Cheryl Ballance, administrative director of the OHC, said if the EMS service was reduced from paramedic-level it would affect all the citizens.
“Of the 103 paramedic calls we had, at least 50 percent originated from the health center,” she said. “We’re here to serve the citizens. (The county providing) health services to the community is so important.”
Leslie Lanier, owner of Books to be Read, testified that it is two and a half hours from Ocracoke to a hospital (via ambulance).
“We’ll be remiss if we go to a lower level of service,” she said. “We have thousands of visitors with anything from a hangnail to a shark attack. We need to get overtime under control, which needs a strong manager.”
At the Monday, Oct. 4 regular meeting, the commissioners again talked about the need to have more solid figures about the true costs and revenues of paramedic-level service vs. a lower level.
At one point, commissioner Anson Byrd said, “Ocracoke is a unique situation. Perhaps we can have basic and intermediate services on the mainland and leave paramedic-level on Ocracoke.”
They commissioners decided to have another special meeting on Oct. 18 to rehash the numbers at 3:30 p.m. before the regular board meeting at 7 p.m.
(Connie Leinbach’s career has included jobs as a daily newspaper journalist and freelancer. She now owns a home on Ocracoke, where she hopes to spend most of her time. She is a reporter for the Ocracoke Observer.)